The care and support
The treatment is a lifelong one, and therefore requires education of you and your family, and then of your child himself, and regular monitoring for an optimal result. In the specific case of phenylketonuria, the diet is often partly relaxed after the age of 10.
This can only be achieved with a mutual investment and trust between you, the parents, and the specialised multidisciplinary medical team that will be in charge of your child’s diet and monitoring, and that will give you all the necessary explanations about the disease.
Medical care
To ensure that your child’s diet is well understood and balanced, regular consultations and blood and/or urine tests will be necessary.
The DOCTOR will monitor your child’s development, biochemical parameters, and the long-term consequences of the disease. He or she will coordinate the care of your child.
The DIETARY, in collaboration with the doctor, will educate you on the diet, and will help you on a regular basis with the choice (quantity and quality) of food for your child according to his/her age. He will adapt the diet according to the biochemical results and your child’s clinical condition.
The BIOCHEMIST will regularly perform plasmaThe liquid part of blood, in which the blood cells are suspended. and/or urine determinations and communicate them to the care team.
The PSYCHOLOGIST, the INSTITUTE and the SOCIAL ASSISTANT will be able to help, in a more general way, to manage the sometimes difficult daily life.
The GENETICIAN can help you to understand the mode of transmission of the disease and can offer you genetic counselling (for subsequent pregnancies) with possibly, for some diseases, the possibility of a prenatal diagnosis.
“Medical, dietary and biochemical monitoring will be essential and adapted according to each pathology and the monitoring methods of each care centre.”
These conditions often lead to constraints that require different types of assistance:
- Family constraints: you will have to “organise” yourself, advice will be given in each chapter according to the circumstances and the age of your child:
- Newborn baby: childcare, eating problems, illnesses,
- Small child: reactions to the diet, starting school,
- Child: family, role of siblings, various celebrations, school, canteen, school trips, holidays, sports…
- Psychological constraints: frustrations due to the treatment, difficulties for you and those around you (family, school, etc.), guilt (due to the hereditary nature of these diseases), must be ruled out. You can call on a psychologist who will see you and your child regularly or according to your needs.
- The psychologist is not there to judge or test you, but to help you and reassure you in the face of a request.
- A psychomotrician and possibly a neurologist will participate in the monitoring and motor evolution of your child.
- A school teacher will possibly carry out a regular assessment of your child’s school achievements and can advise you in the event of school difficulties.
- Social constraints: these conditions are covered at 100% by social security, but in the case of particular problems, a social worker from the hospital service can answer your questions.
Regular exchanges between the medical team and yourself allow the team to get to know your child and his or her environment, so that they can better advise you and help you to balance your child’s illness within his or her own environment and help you to manage daily life.
More information on your treatment guide
Arginine and histidine are semi-indispensable. In fact, only infants need to take them from their food.
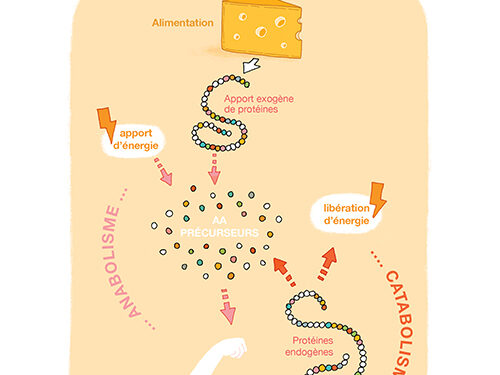
Cysteine, glycine and tyrosine may be indispensable for certain populations catabolism



